


If hip pain is keeping you up at night and making it difficult for you to get up from chairs, stand, walk, or use stairs, a total hip replacement (THR) surgery may be a possible treatment option. The goal of a total hip replacement is to reduce hip pain and improve the motion in your hip.
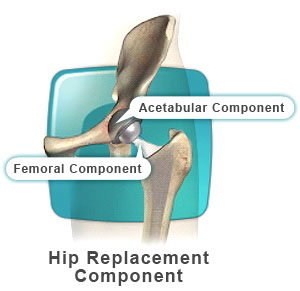
Your hip joint is made up of two parts, the socket, in your hip or pelvic bone and the ball, at the top of your upper leg bone (femur). Your surgeon will make an incision on the side of your thigh and will re-shape the socket to fit the new cup implant that replaces your diseased socket. After the socket is re-shaped, a new cup will be placed in the socket. The cup usually consists of a metal shell and a polyethylene or metal liner. Your surgeon then prepares your femur for the femoral stem, which will hold the new ball part of your hip joint. The head of your femur is removed and the bone is prepared for the new femoral stem. Your surgeon will most likely use a trial implant to verify the correct fit. After your permanent hip stem is implanted, the ball that sits at the top of the femoral stem will be put into place. Once your surgeon is satisfied with the position and movement of your new hip joint, it will be flushed with cleansing fluid and closed with surgical staples.
There are several items to consider when preparing your home for your return from the hospital.
Consider beforehand which entrance you’ll use to access the main living section of your home. The shortest route with the fewest steps will be the entrance of choice. If you have steps into your house, a firm handrail on either or both sides will be of great assistance when you return home. Ensure that lighting is adequate, and be sure there is a clear path from the passenger side of your vehicle to the entrance you’ve chosen.
Several items can be used to increase your level of safety with bathroom needs. For instance, a toilet seat with a low height can be elevated with a raised commode seat to keep your hip from bending too far when sitting. Getting on and off the commode may be easier with the help of handrails or grab bars. Your physical or occupational therapist can help determine the best location of these in a preoperative home safety visit. Having a bed-side commode may be a helpful choice, which will keep you from having to walk all the way to the bathroom in the middle of the night. For accessing your bathtub or shower, you may need one or more grab bars. For additional safety and comfort, be sure to obtain a tub or shower bench. These usually have an adjustable height. When you first try the bench, be sure your knees are positioned slightly below the level of your hips.
To help avoid excessive bending and lifting, arrange your shelves and cupboards with frequently used items at waist to shoulder height. For lighter items that are on lower shelves, be sure to have your reacher handy to keep you from bending over at the hips.
To prevent your hip from bending beyond the ninety-degree limit, you may need to elevate your couch, chair, or recliner. To determine this, try sitting in the various chairs or couches you have in your home that you’ll be sitting in after surgery. Observe whether your knees are positioned above the level of your hips. If so, the surface you are sitting on is too low. A good rule of thumb is to have a seat height that is at least 20 inches above the floor. If you find that your seating arrangement is too low, consider using a platform under the seat or couch to raise it to the desired height. Using 4 x 4 blocks may be helpful, but ensure that the chair or couch is stable when placed on them.
Prepare your floors and hallways by removing throw rugs. Consider rerouting any electrical cords that might be a hazard. Preparing your house in this way may help you avoid a fall due to items that could otherwise catch your foot, causing you to trip or slip. Remove doors that are either too narrow for your walker to fit through or that are heavy and hard to swing open, especially if they separate a frequently used walkway.
Finally, be sure you have good lighting. Overhead and night lighting will be helpful, especially if you need to be up and about at night or other times of low light.
In the weeks before you enter the hospital, your orthopedic surgeon will order tests to make sure you are healthy enough for surgery. Blood tests measure your red blood cell count. An EKG measures your heart. Urine tests in addition to x-rays of the lungs are done. Certain problems like diabetes may slow the healing process so have your complete medical record available.
Also, certain medications like blood thinners and anti-inflammatory medications may result in excessive bleeding and will need to be stopped at a determined time before surgery.
You will then be sent to the recovery room where your health care team will monitor your heart rate, blood pressure, and respiration. You will be given pain medication, which may involve a patient controlled analgesia, which is an IV pain dispenser with a button you control.
The goal of your inpatient hospital stay is to prepare you for discharge from the hospital. During this period all the people involved in your care, your nurse, your therapists, your surgeon and your discharge planner, will meet to discuss your progress and where you should go after the hospital.
Your surgeon will help you decide whether you should return home after surgery or go to an inpatient rehabilitation center.
There are some symptoms you can watch for after surgery. If the surgical area begins to look red, hot, or swollen, and is painful to the touch, this may be the beginning of a blood clot. It is important to seek medical attention immediately if you experience these symptoms. After the surgery, any unusual swelling, redness, warmth or draining of fluid from the hip, especially if you are having fevers, should be reported to your doctor.
Your hip rehabilitation begins right after surgery as ordered by your surgeon. Isometric exercises (tightening muscles without moving the joint) will begin while you are still in bed. You will be instructed to do these exercises a number of times per day. You will be encouraged by the physical therapist to move your ankle and other joints to remain strong.
The usual hospital stay for hip replacement is three to five days. To protect your hip, you will often be asked not to sit past a 90-degree angle after surgery. You will be provided the necessary tools to assist during this process.
The therapist will teach you how to dress, get out of bed without help and use a walker or crutches. You will continue to work to strengthen yourself in preparation for your return home.
It is important for you to follow your doctor’s directions and proper positioning techniques throughout your rehabilitation. By the time you leave the hospital, you should be progressing well in regaining your mobility and stability. If your sutures or clips have to be removed, you will be advised about who will remove them and where this will be done. It is not uncommon to still experience some pain. Remember that full recovery typically takes three to six months.
Just before being discharged, you will receive instructions for your at-home recovery. Until you see the surgeon for your follow-up visit, you should take certain precautions.
Look for any changes around your incision. Contact your surgeon if you develop any of the following:
After undergoing hip replacement surgery, it is important you have realistic expectations about the types of activities you may do.
Driving may be resumed in accordance with the type of surgery you had. If the surgery was performed on your right side, your surgeon may give you permission to drive four to six weeks following surgery. In any case you must be able to move the leg easily from the gas pedal to the brake. If you have a manual shift car and the surgery was on the left side, driving permission may be given at about six weeks following the surgery.
You will be progressed during your physical therapy program from your original walking aid (e.g., walker, crutches) to a cane. Eventually you will use no supportive device as long as there were no other problems encountered requiring long-term use of a walking aid. Eventually you will be allowed to climb stairs step over step. In most cases, patients begin with smaller height steps and gradually progress to standard height steps.
Determining the date you return to work will depend both on your surgeon and the type of work you do. Some individuals may require modifications of their job, while others may easily return to their previous activities. Those engaged in heavy manual labor may have to discuss the possibility of vocational counseling with their surgeon.
There are different risks associated with certain types of leisure and sport activities. Some activities may lead to damage of your artificial joint over time due to wear and tear of the joint. In general, the more vigorous the activity, the higher the risk of damaging the implant, increasing the wear and tear on the implant, or increasing the risk of loosening or dislocating the implant.
Three major categories of activities should be avoided. These include:
Lower stress activities such as golf, hiking, walking, biking, stationary skiing (e.g. Nordic Track), and swimming are excellent forms of exercise for individuals with a hip replacement. Others may also be considered for long-term sports or leisure activities including cross country skiing, doubles tennis, table tennis, and bowling.